5 Simple Tricks to Relieve Annoying Restless Leg Syndrome
Restless Leg Syndrome (RLS), also known as Willis-Ekbom Disease, is a neurological condition that often feels more frustrating than painful but can still be seriously disruptive. Imagine the sensation of needing to move your legs constantly—especially when you’re trying to relax or sleep. For people living with RLS, this urge is not just a fleeting annoyance; it’s a recurring, uncomfortable reality that affects quality of life, sleep, and sometimes even mental health.
What Is Restless Leg Syndrome?
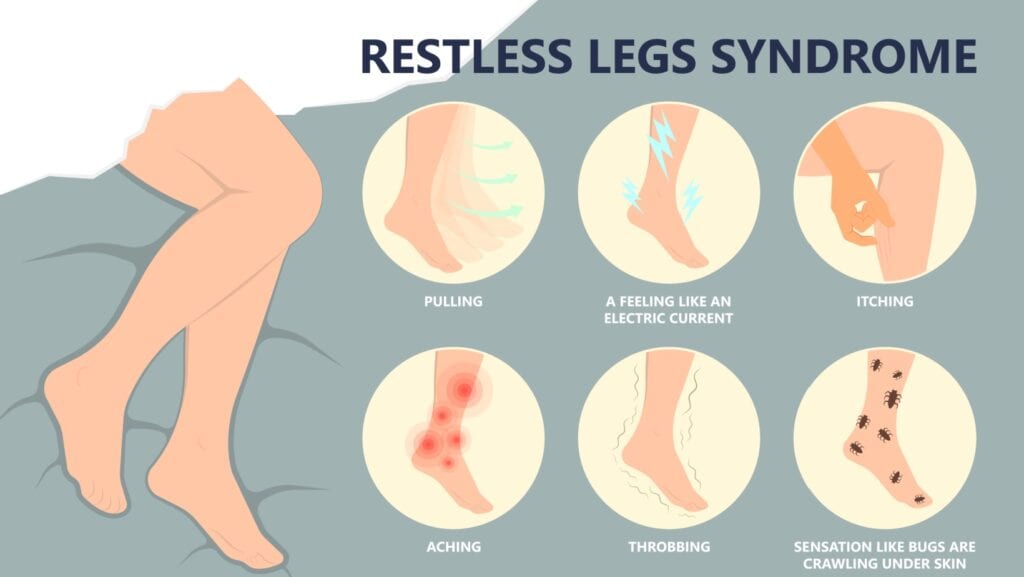
RLS is a condition characterized by an uncontrollable urge to move the legs, usually due to an uncomfortable sensation. The sensations are often described as crawling, tingling, pulling, throbbing, or itching deep in the legs, typically between the knee and ankle. Movement—walking, stretching, or jiggling the legs—temporarily relieves the discomfort, but it usually returns when the person tries to rest again.
Sleep Disturbances

Symptoms often worsen in the evening or at night, which can severely interfere with sleep. According to the National Institute of Neurological Disorders and Stroke (NINDS), sleep disturbances caused by RLS can lead to daytime fatigue, mood issues, difficulty concentrating, and an overall reduction in quality of life
Who Gets RLS?

RLS can affect people of any age, but it’s more common in middle-aged and older adults. Women are more likely to experience RLS than men. According to the Cleveland Clinic, up to 10% of people in the United States may have RLS, although not all cases are diagnosed.
There are two types of RLS: primary and secondary. Primary RLS has no identifiable underlying cause and may be hereditary. Secondary RLS, on the other hand, is usually linked to another medical condition or medication. Some of the common contributors include:
- Iron deficiency or anemia
- Pregnancy, especially in the third trimester
- End-stage renal disease or dialysis
- Peripheral neuropathy
- Certain medications, including antihistamines, antidepressants, and antipsychotics
In fact, studies show that low levels of iron in the brain may contribute to the development of RLS. According to a study in Sleep Medicine Reviews, iron is necessary for proper dopamine function, and dopamine plays a critical role in controlling movement.
How Is RLS Diagnosed?

There is no single test to diagnose RLS. Doctors typically base the diagnosis on a patient’s description of symptoms and medical history. The International Restless Legs Syndrome Study Group has identified five criteria for diagnosis:
- Urge to move the legs, often accompanied by unpleasant sensations.
- Symptoms begin or worsen during periods of rest or inactivity.
- Movement provides partial or total relief.
- Symptoms are worse in the evening or night.
- Symptoms cannot be solely accounted for by another condition.
To rule out other potential causes, your doctor may order blood tests, especially to check iron levels, kidney function, and thyroid hormones.
What Can Be Done?
While there is no cure for RLS, there are a variety of treatment options that can help manage symptoms. The approach often depends on the severity of the symptoms and the presence of any underlying conditions.
1. Lifestyle Changes

For people with mild or intermittent RLS, non-drug approaches can be very effective. These may include:
- Establishing good sleep hygiene: Going to bed and waking up at the same time each day, avoiding screens before bed, and creating a calming bedtime routine.
- Regular exercise: Gentle stretching, yoga, or walking can ease symptoms.
- Avoiding triggers: Limiting caffeine, nicotine, and alcohol.
- Hot baths or leg massages: Can provide short-term relief for many people.
According to the Sleep Foundation, even low-impact exercises like walking and stretching can have a significant impact in reducing RLS symptoms.
2. Iron Supplementation

If tests show low iron levels, iron supplements—either oral or intravenous—may help. According to the the Mayo Clinic, treatment with iron is often the first step when ferritin (a blood protein that stores iron) levels are below 75 ng/mL.
However, supplementation should always be guided by a healthcare provider, as too much iron can be harmful.
3. Medications

For moderate to severe RLS, several medications have been shown to be effective:
- Dopamine agonists, such as pramipexole (Mirapex) and ropinirole (Requip), mimic dopamine in the brain.
- Calcium channel alpha-2-delta ligands, such as gabapentin and pregabalin, can help with nerve pain and sensory symptoms.
- Opioids, like tramadol or oxycodone, may be used in severe, treatment-resistant cases.
- Benzodiazepines, like clonazepam, may be prescribed to aid sleep, though they’re usually a last resort due to dependency concerns.
It’s important to note that some dopamine agonists can lead to a phenomenon called augmentation, where RLS symptoms actually worsen or start earlier in the day. For this reason, medication choices must be carefully managed by a knowledgeable provider.
4. Compression Devices and Vibrating Pads
Some people find relief with pneumatic compression devices or vibrating pads, such as the Relaxis pad, which has FDA clearance for RLS treatment. These devices can be used at night to stimulate the legs and reduce symptoms.
Is RLS Linked to Mental Health?

While RLS is a physical condition, the lack of sleep and chronic discomfort can take a toll on mental health. According to research published in Sleep, people with RLS are significantly more likely to suffer from depression and anxiety. The relationship appears to be bidirectional: poor mental health can exacerbate RLS symptoms, and RLS can worsen mental health, creating a frustrating cycle.
What About Children?

Though often overlooked, RLS does occur in children. Pediatric RLS can be challenging to diagnose, especially because kids may have difficulty describing their symptoms. It may be misattributed to growing pains or behavioral issues. Parents should pay close attention if their child regularly complains of “tickly legs” or frequently gets up and walks around at night.
Conclusion

Restless Leg Syndrome is more than just a quirky urge to move your legs—it’s a legitimate neurological disorder that can disrupt sleep, strain relationships, and reduce quality of life. Fortunately, there are many treatment options available, ranging from simple lifestyle tweaks to targeted medications. If you or someone you know experiences these symptoms, it’s worth bringing it up with a healthcare provider.
The key to managing RLS lies in recognizing the symptoms early, identifying potential triggers or underlying conditions, and working closely with a doctor to find the right treatment plan. With proper support, those living with RLS can take meaningful steps toward better rest—and a better life.
10 Popular Supplements Doctors Wish You’d Stop Taking

READ: 10 Popular Supplements Doctors Wish You’d Stop Taking
Supplements can seem like an easy way to boost your health, but some are unnecessary, ineffective, or even risky. Doctors and nutrition experts often advise against certain widely used products. Here’s a breakdown of ten supplements you might want to rethink before adding them to your routine.
Join Us

Join us on this empowering journey as we explore, celebrate, and elevate “her story.” The Queen Zone is not just a platform; it’s a community where women from all walks of life can come together, share their experiences, and inspire one another. Welcome to a space where the female experience takes center stage. Sign up for our newsletter so you don’t miss a thing, Queen!







