POTS Syndrome: Symptoms, Diagnosis, COVID Link & Why It Affects Women More
Postural Orthostatic Tachycardia Syndrome (POTS) is a condition that many people may have heard of, but few truly understand. It affects the autonomic nervous system and can have a profound impact on daily life, yet it remains underdiagnosed and often misunderstood. Recently, POTS has been thrust into the spotlight due to its association with long COVID, sparking curiosity and concern.
This article explores what POTS is, how it is diagnosed and treated, why it disproportionately affects women, its relationship to COVID-19, and why it has become a topic of increasing conversation.
What Is POTS?

POTS is a disorder of the autonomic nervous system, which regulates involuntary bodily functions such as heart rate, blood pressure, and digestion. It is characterized by an excessive increase in heart rate when transitioning from a lying or sitting position to standing. Specifically, individuals with POTS experience a heart rate increase of 30 beats per minute or more (or over 40 beats per minute in adolescents) within 10 minutes of standing, without a significant drop in blood pressure.
Symptoms of POTS extend beyond tachycardia and can include dizziness, fainting, fatigue, brain fog, nausea, and difficulty exercising. These symptoms can severely impact daily life, making simple tasks like standing in line or showering a challenge.
How is POTS Diagnosed?

Diagnosing POTS can be challenging due to the wide range of symptoms and overlap with other conditions. A thorough medical history and physical examination are essential. The diagnosis typically involves:
- Tilt Table Test: This is the gold standard for diagnosing POTS. During the test, the patient is strapped to a table that tilts them from a horizontal to a vertical position while their heart rate and blood pressure are monitored.
- Active Stand Test: This simpler alternative involves measuring heart rate and blood pressure while the patient moves from lying down to standing.
- Exclusion of Other Conditions: Doctors often rule out other potential causes of symptoms, such as dehydration, anemia, thyroid disorders, or adrenal insufficiency.
- Additional Tests: Depending on the patient’s symptoms, doctors may recommend blood tests, autonomic function tests, or imaging studies.
How is POTS Treated?

There is no cure for POTS, but several treatment strategies can help manage symptoms. These include:
Lifestyle Modifications

There are lifestyle modifications that you can take:
- Increased Fluid and Salt Intake: Many POTS patients benefit from drinking 2-3 liters of fluids daily and increasing their salt intake to improve blood volume.
- Compression Garments: Wearing compression stockings or abdominal binders can help reduce blood pooling in the legs.
- Exercise: A structured, gradual exercise program focusing on recumbent exercises (like swimming or cycling) can improve symptoms over time.
Medications

Speak with your doctor about potentially helpful medications:
- Beta-Blockers: To help regulate heart rate.
- Fludrocortisone: To increase blood volume.
- Midodrine: To improve blood vessel constriction.
- Ivabradine: To reduce heart rate.
- Other Medications: Depending on specific symptoms, drugs targeting migraines, anxiety, or gastrointestinal issues may be prescribed.
Dietary Changes

Eating smaller, more frequent meals and avoiding large meals or those high in carbohydrates can help.
Cognitive Behavioral Therapy (CBT)
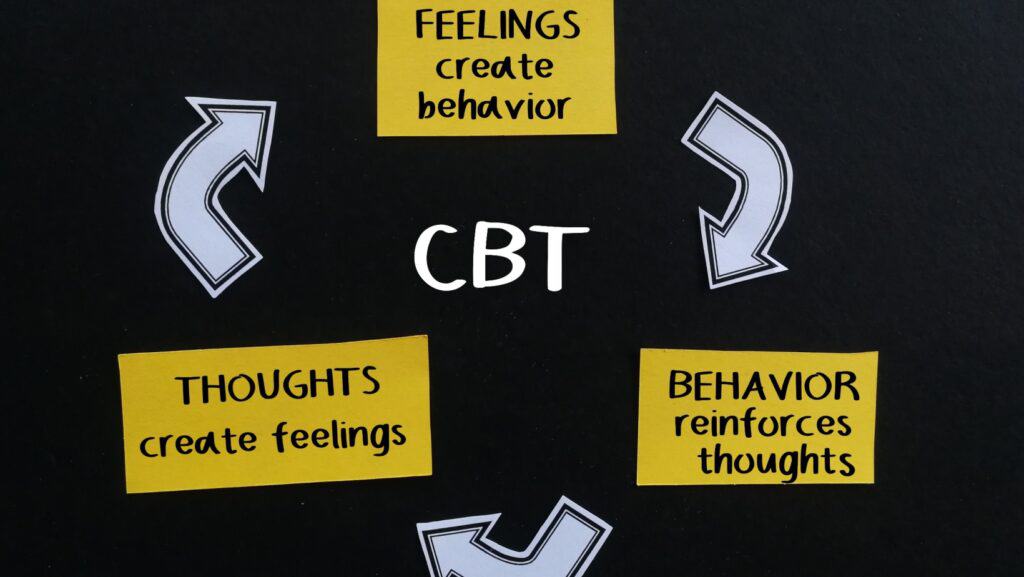
In some cases, CBT may be beneficial for managing the emotional and psychological impacts of living with POTS.
Why Do More Women Get POTS?

POTS disproportionately affects women, with approximately 80% of patients being female. While the exact reason for this gender disparity is not fully understood, several factors may contribute:
- Hormonal Influences: Fluctuations in estrogen and progesterone levels, such as during the menstrual cycle, pregnancy, or menopause, may exacerbate symptoms.
- Autoimmune Link: Women are more likely to develop autoimmune diseases, which are sometimes associated with POTS.
- Structural Differences: Studies suggest that women may have different autonomic responses or vascular structures that could predispose them to POTS.
You may want to read: Why Autoimmune Diseases Disproportionately Affect Women
The Relationship Between POTS and COVID-19

Since the onset of the COVID-19 pandemic, a significant increase in POTS diagnoses has been observed. Many of these cases are linked to long COVID, a condition characterized by lingering symptoms following a COVID-19 infection. Researchers believe that the SARS-CoV-2 virus may trigger POTS through:
- Autonomic Nervous System Damage: The virus may directly or indirectly damage the autonomic nervous system.
- Immune System Dysregulation: The immune response to COVID-19 can lead to chronic inflammation, which may play a role in POTS development.
- Precipitation of Autoimmune Disorders: COVID-19 may trigger or exacerbate autoimmune conditions that are associated with POTS.
This link has highlighted the need for increased awareness and research into POTS and its management in the context of post-viral syndromes.
Why Am I Hearing More About POTS Recently?

POTS has moved from relative obscurity to mainstream discussion for several reasons:
- COVID-19 Pandemic: As mentioned, the surge in long COVID cases has brought attention to POTS as a potential post-viral complication.
- Increased Awareness: Advocacy from patients, healthcare providers, and organizations like Dysautonomia International has led to greater recognition of POTS in both the medical community and the public.
- Advances in Research: Ongoing studies are shedding light on the underlying mechanisms of POTS and its treatment, leading to improved diagnostic and therapeutic approaches.
- Social Media and Online Communities: Patients have taken to platforms like Twitter, TikTok, and Facebook to share their experiences, raising awareness and fostering a sense of community among those affected.
- Celebrity Advocacy: Public figures and celebrities who have shared their struggles with POTS have helped bring attention to the condition.
- Diagnostic Improvements: With better diagnostic tools and increased clinician education, more cases of POTS are being accurately identified.
Conclusion

POTS is a challenging condition that affects many aspects of life but is becoming increasingly understood and recognized. Whether through advances in diagnosis, management strategies, or heightened awareness due to the COVID-19 pandemic, individuals with POTS are finding more support than ever before. While much remains to be learned, the spotlight on POTS offers hope for improved treatments and outcomes for those affected by this complex syndrome.
Hypertension Risk: Early Signs Of This Silent Killer

Hypertension, commonly known as high blood pressure, is often referred to as the “silent killer.” This term underscores its insidious nature; the condition frequently develops without noticeable symptoms, yet it poses significant risks to overall health. Affecting nearly half of adults in the United States, hypertension is a major public health concern worldwide. This article explores what hypertension is, its causes, symptoms, complications, and strategies for prevention and management.
READ: Hypertension Risk: Early Signs Of This Silent Killer
Join Us

Join us on this empowering journey as we explore, celebrate, and elevate “her story.” The Queen Zone is not just a platform; it’s a community where women from all walks of life can come together, share their experiences, and inspire one another. Welcome to a space where the female experience takes center stage. Sign up for our newsletter so you don’t miss a thing, Queen!







